A topic that arises frequently in our discussions with pain physicians is the use of ketamine to treat chronic pain. Many doctors have incorporated ketamine into their treatment regimens for chronic pain, while others are exploring its benefits, either intrathecally or intravenously. We discuss the latter in this article, since it appears to be the dominant method of delivery between the two. We will, however, be sure to circle back to ketamine in a future newsletter to discuss its utilization within targeted drug delivery systems.
Background
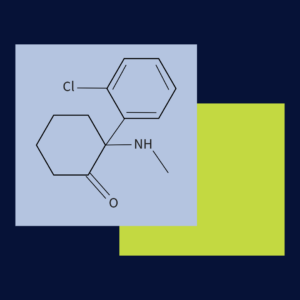
Ketamine hydrochloride, approved by the FDA in 1970, acts primarily as a noncompetitive antagonist of the N- methyl-D-aspartate (NMDA) receptor for glutamate. It is a major excitatory neurotransmitter within the central nervous system. Ketamine was originally indicated as an anesthetic induction agent, with doses ranging from 1mg/kg to 4.5mg/kg. It exists in two enantiomers: S & R structures. The S enantiomer has greater potency due to its affinity for the PCP binding sites on the NMDA receptor. Structurally related to phencyclidine, ketamine has a lower incidence of hallucinations and minimal effect on respiratory function. Some studies suggest ketamine desensitizes excitatory receptor systems within the CNS. It can, however, produce a dissociative sensation that some individuals exploit for non-medical use cases. Other reported effects include elevated blood pressure (as opposed to most anesthetics), and bronchodilation1. Over the past two decades, however, ketamine has gained much traction in the treatment of chronic pain.
Ketamine for Chronic Pain
Use cases for ketamine are wide ranging. Studies dating back to the 1990s suggest that IV ketamine infusions are effective in reducing pain in Complex Regional Pain Syndrome (CRPS), and may also prove useful for other chronic pain syndromes that involve central sensitization, including postherpetic neuralgia, migraine, burns, fibromyalgia, as well as neuropathies1234 . One particular study by Sigtermans et al treated patients for 4 days with a 22 mg/h/70 kg infusion. The patients experienced significantly lower pain scores over a 12-week evaluation period. A longitudinal study by Sheehy et al, observed significant pain relief in children and adolescents suffering from chronic pain. The patients were infused for 3 days with 0.3 mg/kg/h for 4 hours to 8 hours. The ketamine treatment showed greater pain reduction scores with CRPS than previous treatments. Lastly, Swartzman et al performed a double blind randomized controlled study treating patients with ketamine 0.35 mg/kg/hr infused over 4 hours for 10 days. The maximum dose administered was 25mg/hr for 4 hours. Patients were initially evaluated 2 weeks prior to treatment, with a follow up performed after 3 months. This study demonstrated significant reduction in many pain parameters for up to 90 days5. I have spoken with clinicians who are administering doses of ketamine ranging from 50 to 800mg per treatment. Their clinical opinion is that it has proven to be effective at reducing chronic pain.
Working With Ketamine
I became aware of ketamine infusions in 2000 and, in order to learn more, I sought out physicians utilizing it for chronic pain. The infusion process and its lasting pain relief effects intrigued me. Though ketamine is a well-established analgesic agent, I have witnessed a noticeable uptick in inquiries from physicians interested in ketamine outside of the operating room. This appears to be playing out in the proliferation of ketamine infusion clinics across the country. I offer some considerations for beginning ketamine IV therapy. As stated, you will need a dedicated setting for treatment of patients with ketamine due to incidences of hallucination and dissociative sensations. I would recommend hiring registered nurse or other similar personnel with IV therapy experience. Some supplies will be necessary such as: IV cannulas (22 – 24G), or butterfly needles of similar gauge, IV tubing, IV piggyback (100- 250ml), monitoring equipment and medicines for treating side effects. I strongly encourage you to determine if medical insurance will cover such therapy and reimbursement is appropriate. Based on conversations with various physicians, patient may be willing to pay cash if insurance coverage is non-existent.
Ketamine appears to have built for itself a reputation for being the pharmaceutical gift that keeps on giving. Today, due to its growing popularity, data on it’s benefits to patients suffering from a wide variety of conditions continues to mount. And more benefits are being studied! It is a pharmaceutical with a long and storied history which has, at times, involved illicit abuses. I’m reminded of a particular scene in Armageddon during which a NASA-employed physician implies that Ketamine, which was identified in the prospective astronauts’ blood samples, is a sedative to be utilized only on large animals, specifically horses. While certainly an effective analgesic, I hope this discussion has served to take some of the drama out of the subject of IV ketamine infusions.
If you would like to have an extended conversation related to ketamine; my door is open if questions arise. Thank you for this opportunity to present this information.
- https://academic.oup.com/painmedicine/article/20/2/323/4925560
- https://academic.oup.com/painmedicine/article/16/5/943/2460721
- https://link.springer.com/article/10.1007/s11916-018-0664-x
- https://pubs.asahq.org/anesthesiology/article/133/1/13/109071/Ketamine-for-Chronic-PainOld-Drug-New-Trick
- https://pubmed.ncbi.nlm.nih.gov/34820225/


Leave A Comment